Wednesday, January 4, 2012
Tuesday, January 3, 2012
Tuesday, January 3rd
Trying to get it together before the surgery tomorrow. I have a checklist of pre-surgery instructions:
· No food or drink after midnight
· No shaving in the area of the surgery
· Bathe the night before and morning of surgery with supplied anti-septic soap
I have a small travel bag packed with a pair of PJ’s, and shave kit for Momma to bring when I’m able to get up and move around. I’ll have family with me before and after the surgery, so lots of prayers and comfort knowing they’re close.
My single largest trepidation is the pain meds. I have a real problem with aspirin based pain meds and don’t want to go through the nausea again, especially in the hospital! As for fears of complications with the surgery, I’ve read a lot of good and a lot of bad and don’t want to dwell on the negative, so staying positive. Got to say I’m anxious to get off the Diamox!
Monday, January 2, 2012
Monday, January 2nd
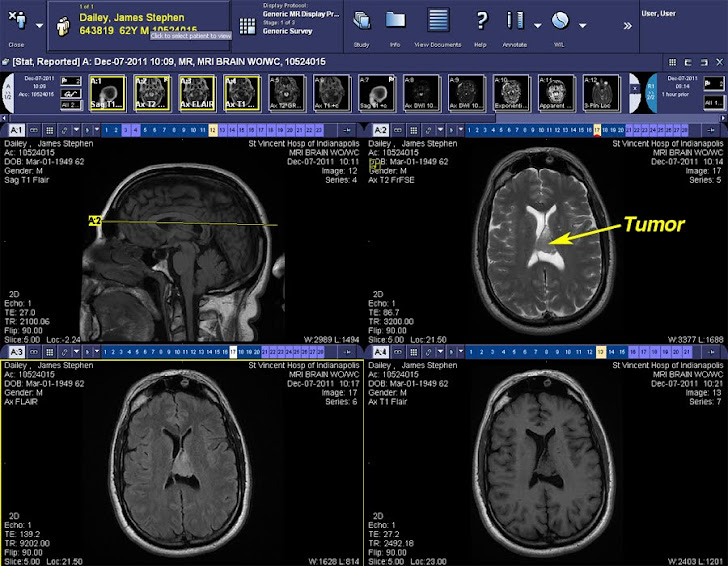
Been getting a little nervous about the surgery. The neurosurgeon gave me a brochure describing the procedure, but it wasn't very descriptive. So, off to the World Wide Web to get the low down. This was one of the best descriptions, while not the exact location, it does convey the general procedure well. This information is courtesy of the Mayfield Clinic.
What happens during surgery?
There are 6 main steps during a craniotomy. Depending on the underlying problem being treated and complexity, the procedure can take 3 to 5 hours or longer.
Step 1: prepare the patient
No food or drink is permitted past midnight the night before surgery. Patients are admitted to the hospital the morning of the craniotomy. With an intravenous (IV) line placed in your arm, general anesthesia is administered while you lie on the operating table. Once asleep, your head is placed in a 3-pin skull fixation device, which attaches to the table and holds your head in position during the procedure (Fig. 2). Insertion of a lumbar drain in your lower back helps remove cerebrospinal fluid (CSF), thus allowing the brain to relax during surgery. A brain-relaxing drug called mannitol may be given.

Figure 2. The patient’s head is placed in a three-pin Mayfield skull clamp. The clamp attaches to the operative table and holds the head absolutely still during delicate brain surgery. The skin incision is usually made behind the hairline (dashed line).
Step 2: make a skin incision
After the scalp is prepped with an antiseptic, a skin incision is made, usually behind the hairline. The surgeon attempts to ensure a good cosmetic result after surgery. Sometimes a hair sparing technique can be used that requires shaving only a 1/4-inch wide area along the proposed incision. Sometimes the entire incision area may be shaved.
Step 3: perform a craniotomy, open the skull

Figure 3. A craniotomy is cut with a special saw called a craniotome. The bone flap is removed to reveal the protective covering of the brain called the dura.
Step 4: exposure the brain
After opening the dura with surgical scissors, the surgeon folds it back to expose the brain (Fig. 4). Retractors placed on the brain gently open a corridor to the area needing repair or removal. Neurosurgeons use special magnification glasses, called loupes, or an operating microscope to see the delicate nerves and vessels.

Figure 4. The dura is opened and folded back to expose the brain.
Step 5: correct the problem
Because the brain is tightly enclosed inside the bony skull, tissues cannot be easily moved aside to access and repair problems. Neurosurgeons use a variety of very small tools and instruments to work deep inside the brain. These include long-handled scissors, dissectors and drills, lasers, ultrasonic aspirators (uses a fine jet of water to break up tumors and suction up the pieces), and computer image-guidance systems. In some cases, evoked potential monitoring is used to stimulate specific cranial nerves while the response is monitored in the brain. This is done to preserve function of the nerve and make sure it is not further damaged during surgery.
Step 6: close the craniotomy

Sunday, January 1, 2012
Sunday, January 1st, 2012
Happy New Year!
The good news, there is no news! Been sleeping well, mild headaches but easily managed without meds. Still lethargic, still have the loss of appetite, but no changes.
I did speak with the pre-surgical exam doctor and forgot to include the conversation in my last post. She called to say the increased red cell count was caused by the Diamox, and that she had added a note to my folder that I was intolerant to aspirin based pain meds.
T-minus 68 hours and counting!
Subscribe to:
Posts (Atom)